How Hospitals End the Turnover Cycle: Nurse Retention Strategies That Work
High nurse turnover is one of the most urgent threats health system leaders face today. When experienced nurses walk out the door, the impact ripples across the entire organization. Budgets tighten under the weight of recruitment costs and agency spending. Patient care teams lose continuity and cohesion. Quality metrics and patient satisfaction can slip.
For many health systems, short-term coverage solutions, from overtime to agency labor, have become the go-to response to workforce shortages. While these quick fixes help plug immediate gaps, they often create deeper structural problems over time. Burnout intensifies. Labor costs steadily climb. Team cohesion weakens. And eventually, the patient experience begins to suffer.
The most resilient organizations take a different approach. Rather than constantly chasing short-term coverage, they invest in nurse retention strategies that strengthen their workforce for the long haul—building stability, continuity, and sustainability into the system itself.
Recommended Reading: 5 Nurse Retention Strategies for Supporting Gen Z
Building a Resilient Nursing Workforce: Roles That Support Retention
Healthcare workforce resilience starts with aligning your workforce to real-time clinical demand and supporting nurses with flexible employment options that meet organizational needs and individual preferences.
Core Nursing Staff: The Foundation of Stability
Permanent, full-time nurses form the backbone of any resilient health system. They provide continuity, clinical expertise, and institutional knowledge that anchor patient care and team operations. Engaged core nurses mentor newer staff, strengthen interdisciplinary collaboration, and help maintain cultural continuity across the organization.
When core nurses feel supported, units run more efficiently, communication improves, and patients experience more consistent care. Effective retention strategies prioritize investing in and protecting this group, rather than stretching them thin to fill systemic coverage gaps.
PRN Nurses: Flexible Coverage That Reduces Burnout
PRN nurses are a strategic tool for healthcare workforce sustainability. By offering flexible schedules that align with organizational needs and individual preferences, PRN nurses provide coverage without overburdening core nurses.
This flexibility helps prevent burnout, supports work-life balance, and ensures that units remain fully staffed during holidays, weekends, or seasonal surges. Used thoughtfully, PRN nurses contribute to nurse satisfaction and long-term retention.
Float Pool Nurses: Versatile Support for Consistent Care
Float pool nurses add a dynamic layer of support to the workforce. Unlike PRN employees, float pool nurses are scheduled employees who can move across units to fill gaps and respond to fluctuations in patient volume.
By strategically deploying float pool nurses, hospitals balance workloads, maintain continuity of care, and relieve pressure on permanent employees. This adaptability ensures that patient care standards remain high, even during busy periods, and strengthens overall workforce resilience.
Recommended Reading: How to Build a Nurse Float Pool for Fast, Cost-Effective Shift Fulfillment
On-Demand Clinicians: Rapid Response Without Sacrificing Stability
Local on-demand clinicians provide immediate coverage for urgent or unplanned coverage needs. When deployed thoughtfully, they protect core nurses from excessive overtime, maintain safe staffing ratios, and ensure patient care continues uninterrupted.
Far from being temporary, on-demand clinicians are a critical part of a layered workforce strategy that supports stability, reduces burnout, and reinforces a sustainable workforce model.
Recommended Reading: Resilient Health System Workforce Planning

Advanced Workforce Technology: Enabling Smarter Staffing Decisions
Creating diversified employment pathways is only half the solution when it comes to long-term workforce planning. To truly unlock workforce resilience, organizations also need advanced workforce technology that eliminates time-consuming manual scheduling and automates assignments based on forecasted patient demand, while factoring in individual skills, experience, and scheduling preferences.
Many health systems are now incorporating intelligent open shift management into their workforce operations, allowing available shifts to be posted and filled quickly and cost-effectively based on pre-defined qualifications and rules.
For nurse managers, this shift is transformative. Many still rely on spreadsheets and manual coordination to manage call-outs and balance schedules—tasks that consume time and create daily frustration. In fact, recent survey data shows that 39% of nurse leaders cite managing call-out coverage as a primary source of stress, while 26% struggle with the complexity of building and balancing staff schedules.
By integrating workforce demand forecasting, real-time data visibility, customizable scheduling tools, and predictive staffing algorithms, organizations can significantly improve operational efficiency. This data-driven approach enhances scheduling accuracy and labor cost control while also promoting nurse autonomy and supporting better work-life balance.
When implemented effectively, advanced workforce technology streamlines operations and strengthens nurse retention by creating a more predictable, transparent, and supportive environment.
A Look at Real-World Nurse Retention Strategies
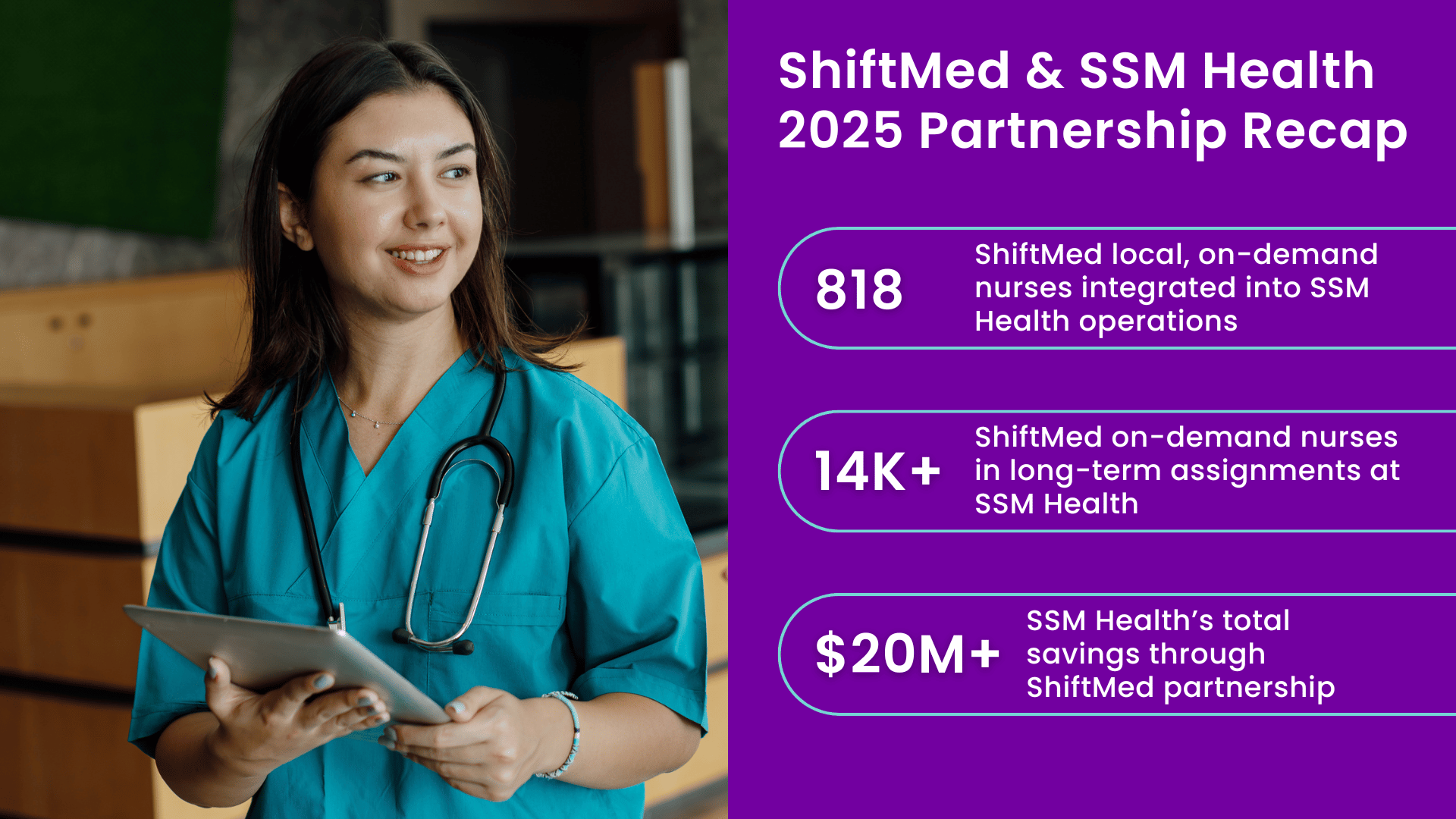
Incorporating flexible nursing staff and advanced workforce technology isn’t just a theoretical strategy. Leading health systems, including Missouri-based SSM Health, have implemented long-term workforce planning supported by ShiftMed and achieved measurable improvements in financial and clinical performance.
By prioritizing scheduling autonomy, work-life balance, and data-driven decision-making, SSM Health has shifted from reactive coverage to a more predictable, centralized workforce model. Demand forecasting and diversified employment pathways have improved scheduling accuracy, reduced reliance on premium labor, and lowered burnout-related nurse turnover.
The result is more than just better shift coverage; it’s a sustainable workforce infrastructure that strengthens retention, improves labor cost control, and supports high-quality patient care, proving that workforce resilience is an operational and financial advantage.
ROI of Long-Term Workforce Planning
SSM Health’s experience underscores a broader reality: long-term workforce planning delivers measurable return on investment.
While retention strategies require upfront commitment, the financial impact compounds over time. Lower turnover reduces recruitment, onboarding, and training costs. A more stable workforce decreases overtime spending and limits reliance on premium agency labor. At the same time, improved morale and scheduling predictability enhance productivity and reduce absenteeism.
For financial and operational leaders, sustainable nurse retention strategies are structural cost-control mechanisms that protect margins while strengthening care delivery.
Metrics That Define Workforce Resilience
Achieving workforce resilience requires disciplined measurement. Leading health systems track a defined set of workforce indicators to monitor stability and guide decision-making, including:
Nurse turnover rate
Average nurse tenure
Overtime utilization
Agency labor percentage
Correlations between staffing stability and patient outcomes
Consistent monitoring of these metrics enables leadership teams to identify pressure points early, proactively adjust workforce models, and prevent minor disruptions from becoming systemic instability.
Implementing Retention-Focused Workforce Design
Designing for retention requires intentional action at the leadership level. Sustainable workforce models aren’t built through isolated initiatives; they’re embedded into operational strategy.
Start with a Clear Workforce Assessment
Effective change begins with visibility. Leaders must understand where instability exists and why. Start by asking these questions:
How reliant is the organization on temporary or premium labor?
Where are overtime spikes most frequent?
Which units experience the highest turnover or engagement challenges?
A comprehensive workforce assessment often reveals whether short-term coverage solutions have become structural dependencies. Clarity at this stage creates the foundation for meaningful, system-level redesign.
Invest in Professional Growth and Engagement
Nurse retention strengthens when clinicians see a future within the organization. For example, structured mentorship, clear clinical advancement pathways, leadership development, and ongoing education signal a long-term commitment to the workforce. When nurses feel supported, valued, and empowered to grow, loyalty increases, and turnover decreases.
Prioritize Wellbeing as an Operational Strategy
Burnout remains one of the strongest predictors of nurse turnover. Resilient health systems address this proactively by embedding wellbeing into workforce design. This includes access to mental health resources, flexible scheduling options, appropriate nurse-to-patient ratios, and adequate recovery time between shifts. These measures protect clinical performance and workforce stability.
Measure, Refine, and Scale
Retention-focused workforce design is an ongoing operational discipline. Leading organizations continuously monitor key workforce metrics, analyze trends, and refine staffing models accordingly. Successful pilots are scaled. Emerging risks are addressed early. Strategies evolve as workforce dynamics change. Through consistent evaluation and adjustment, workforce resilience becomes embedded in an organization’s operating model.
Conclusion: Nurse Retention Strategies as a Strategic Advantage
Nurse retention strategies are no longer optional; they’re a critical organizational priority. Health systems that integrate core staff, PRN nurses, float pools, and on-demand clinicians with advanced workforce technology create flexible, sustainable workforce models.
Long-term workforce planning goes beyond filling shifts. It reduces turnover, lowers labor costs, improves care quality, and strengthens team engagement. As SSM Health demonstrates, organizations that combine centralized staffing, diversified employment pathways, predictive scheduling, and professional development see measurable improvements in financial performance, operational efficiency, and nurse satisfaction.
For hospital leaders, the message is clear: workforce resilience is not just a cultural initiative — it is a strategic advantage. By embedding retention-focused strategies into operational design, leaders can protect margins, enhance patient outcomes, and ensure their teams are equipped to thrive today and into the future.