ShiftMed Innovation Summit Unveils Bold Workforce Strategies Shaping the Future of Healthcare
The future of healthcare won’t wait—and neither should your workforce strategy. At the ShiftMed 2025 Workforce Innovation Summit in New York City, leaders from top health systems explored how innovative workforce models are transforming care delivery. The decisions health systems make today will determine who thrives and who risks falling behind.
4 Critical Conversations Redefining the Healthcare Workforce
The future of healthcare work was distilled into one question: how do hospitals create a workforce that flexes, performs, and endures? Leaders pointed to actionable solutions—reimagined nurse scheduling, AI-powered workflows, and interoperability at scale—already transforming hospital operations.
1. Flexible Nurse Scheduling Options for Health Systems
Traditional workforce strategies are failing today’s nurses. Health systems must embrace flexible nurse scheduling as a strategic imperative to retain top talent, optimize patient care, and protect financial performance.
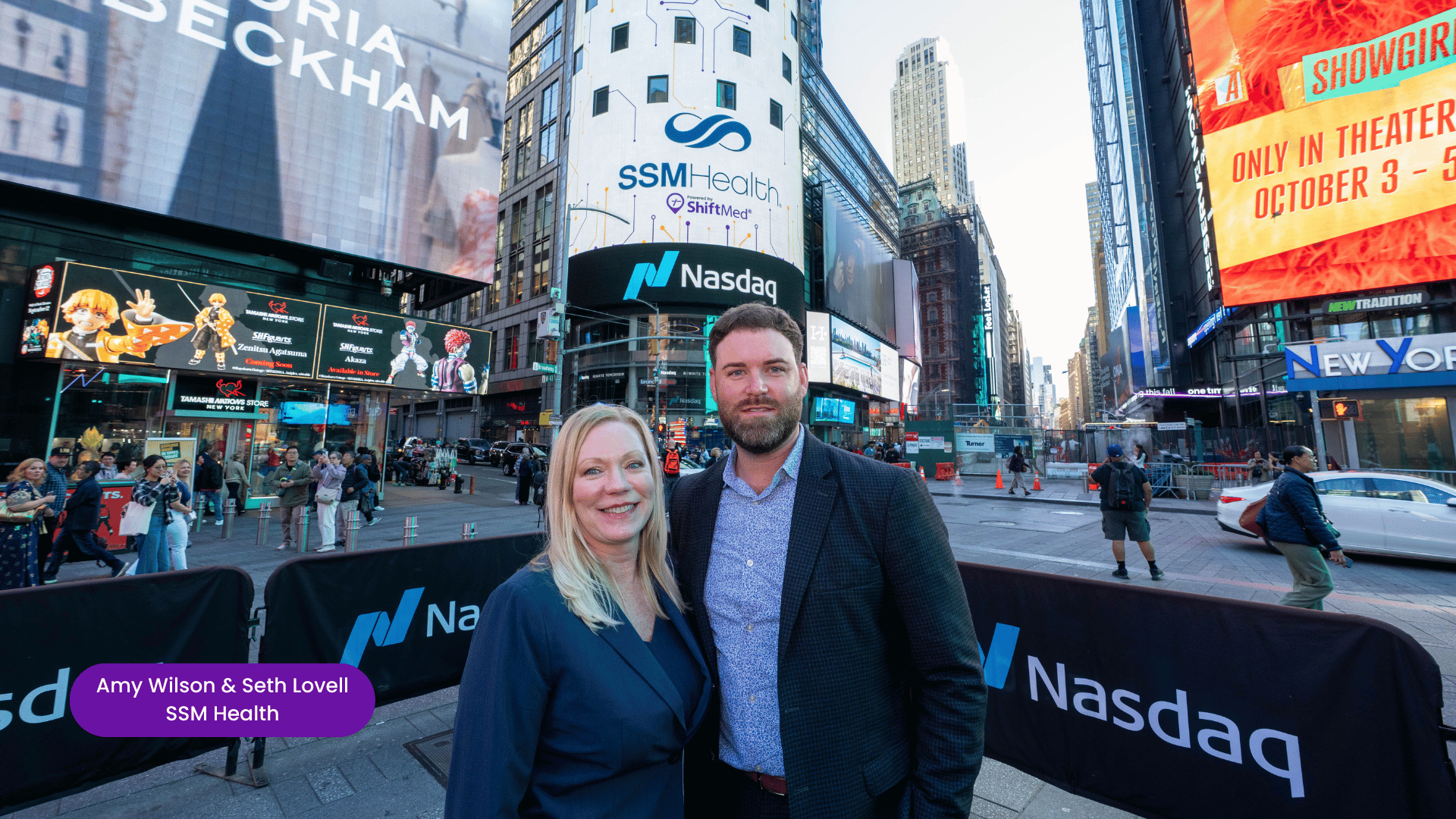
At the summit, Seth Lovell, System Vice President of Nursing Transformation and Innovation at SSM Health, was asked whether health systems will attract top talent through pay, culture, or flexibility. He emphasized that flexibility is emerging as the key driver for nurses.
Lovell explained that historically, nurses prioritized hourly pay, then shifted their focus to total compensation and benefits. Today, flexibility has taken the lead, and looking ahead, the next priority will be workload burden. Health systems must consider how much support nurses have, the quality of their work environment, and how optimized their day-to-day is through technology, robotics, and AI. He concluded that while pay, benefits, and flexibility remain important, addressing workload and operational efficiency will ultimately define the future of nurse satisfaction.
Building on Lovell’s point, his colleague Amy Wilson, System Chief Nurse Executive at SSM Health, highlighted the importance of defining flexibility. She explained that flexibility is in the eye of the beholder and looks different for every nurse, so health systems need to offer a menu of options to meet nurses where they are at various points in their lives.
Kelley Strandberg, ShiftMed VP of Nursing and Workforce Innovation, echoed this perspective, emphasizing the role of technology in supporting flexibility. “I think flexibility and technology will drive the future of healthcare. Pay gets nurses in the door, but flexibility keeps them. Nurses across all generations—especially Gen Z—are not just asking for it, they’re demanding it. We’re seeing the rise of four-day workweeks and mental health days; all tied to flexible offerings. That’s what will shape retention moving forward.”
Technology, such as self-scheduling apps, is critical in enabling this flexibility. Todd Walrath, ShiftMed CEO, noted that health systems often wait to adopt new technology until it’s proven. However, being an early adopter pays off regarding flexible workforce solutions. Health systems that offer flexible work options first can attract part-time nurses and other staff before competitors do, tapping into local talent that might otherwise go elsewhere. Therefore, early adoption allows organizations to fill more shifts efficiently and gain a competitive advantage in their market, securing the best workforce before anyone else.
2. Adopting AI for Clinical Workflows
During the summit, Joanne Laguna-Kennedy, Chief Operating Officer at Cedars-Sinai, was asked what she sees as the biggest disruptor to traditional shift fulfillment models over the next three years. She pointed to technology—especially AI—as the most transformative force, noting that the healthcare industry has historically been slow to adopt innovation.
AI is already proving its potential to make clinical workflows faster, easier, and more precise. By analyzing skills, experience, and facility needs, AI can match clinicians to the right units, provide real-time scheduling recommendations, fill staffing gaps instantly, and reduce costs by minimizing mismatches and streamlining operations.
ShiftMed COO Jacob Laufer said, “I think embracing AI for shift routing will be a game changer. Filling an ICU shift is incredibly complex for unit managers today, and AI can simplify that process. Clinicians want flexibility, hospitals need oversight, and both sides benefit from smarter, more efficient scheduling that supports better patient outcomes.”
The impact of AI in healthcare is already measurable. According to a Deloitte workforce technology study, generative AI and automation can reduce the time revenue cycle teams spend by up to 50%, while giving bedside nurses up to 20% more time to focus on direct patient care.
3. Taking Smart, Strategic Risks
Bold workforce strategies were a central focus throughout the summit. When asked about the most ambitious approach for driving results, ShiftMed’s Jacob Laufer highlighted position control processes as a major opportunity.
“Hospitals have the chance to take smarter, strategic risks with overtime and pay policies, carefully balancing them against local market demands,” he explained. “This is the sweet spot everyone is trying to figure out—how to manage full-time and part-time dynamics while meeting the expectations of today’s workforce.”
Another innovative approach to gaining attention is search-based incentive pay for nurses. Ashley Foster, ShiftMed Executive VP of Acute Partnerships, sees it as a game-changer for managing high-demand surge staffing.
“It’s risky because it borrows from the gig economy and can be challenging for CFOs, but it has huge potential,” she said. Unlike traditional bonuses, this strategy uses predictive modeling to incentivize clinicians to pick up shifts early. Some models even explore a bid-based system where nurses can set their own rates. “These are bold ideas, but they represent the type of workforce innovation that will define the future of healthcare staffing,” Foster added.
4. Improving Interoperability in Healthcare Staffing
Managing a clinical workforce across disconnected systems creates delays, confusion, and inefficiency. So, when ShiftMed’s Kelley Strandberg was asked what she would change about how health systems integrate their workforce operations, her answer was clear: “If I could change one thing, it would be for them to focus on true interoperability. Managers shouldn’t have to juggle 10 different platforms to manage their workforce. The future lies in a single, integrated source of truth—one platform that unifies data, simplifies operations, and drives smarter decisions.”
The Time for Bold Healthcare Workforce Strategies Is Now
A clear consensus emerged from the summit: healthcare’s future workforce will be built on the balance of technology, trust, and flexibility. Download the white paper to uncover how health system leaders are redefining leadership visibility, flexibility, and technology to create a more resilient workforce.