How to Master Float Pool Management in Hospitals

Effective hospital float pool management is a powerful lever for healthcare workforce efficiency. When float nurses are properly resourced and empowered to practice at the top of their scope, they deliver measurable cost savings, greater staffing flexibility, and improved operational performance. Yet without strategic oversight, float pools can quickly become underutilized, leading to higher turnover, staffing instability, and compromised care quality.
So why aren’t more hospitals maximizing this critical resource? In many cases, the barriers are structural. Decentralized scheduling systems limit visibility and coordination. A lack of real-time data makes it difficult to deploy staff where and when needed. Inconsistent onboarding can leave float nurses underprepared and managers hesitant to use them across units.
The result? Underused nurse float pools that drain internal resources, drive up labor costs, increase burnout, and put patient coverage at risk. The solution lies in a more strategic approach that leverages the right systems, support, and structure to make the float pool an indispensable part of a hospital's workforce strategy.
Why Nurse Float Pools Are the Future
Despite progress in post-pandemic workforce recovery, the nursing shortage remains a critical challenge. The U.S. Department of Health and Human Services projects a persistent shortfall of full-time RNs—estimated at a 10% gap by 2027 and 6% by 2037—leaving nearly 208,000 essential roles unfilled nationwide.
In this environment, optimizing your float pool is a strategic imperative. A well-managed float pool unlocks a flexible, cost-efficient clinical resource that strengthens shift coverage, cuts agency spend, and boosts nurse engagement. Health systems that fail to invest in float pool growth and optimization now risk escalating labor costs, rising turnover, and falling behind more adaptive, strategically aligned competitors.
Hospitals that utilize float pools as part of an overall workforce management plan typically save 2% to 5% on total nursing labor costs.
3 Ways Flexible Scheduling Fuels Float Pool Growth
Flexible scheduling is a powerful tool for expanding and sustaining an effective nurse float pool. By giving nurses greater control over when and where they work, hospitals can boost engagement, tap into a wider labor pool, and reduce turnover. Here are three key ways flexible scheduling supports float pool growth and performance.
1. Provides Work-Life Balance
Many nurses—particularly millennials, Gen Z, and those re-entering the workforce—prioritize flexibility and work-life balance. Offering self-scheduling options makes float pool roles significantly more attractive than rigid, fixed shifts. When nurses have control over when and where they work, they’re more likely to pick up open shifts, reducing overtime, lowering dependence on agency staff, and improving unit coverage.
2. Enables Per Diem Participation
Not every qualified nurse can commit to a full-time role. Many are balancing school, caregiving responsibilities, or personal obligations that limit their availability. Flexible scheduling allows part-time and per diem nurses to meaningfully contribute through float pools. By allowing them to choose shifts that align with their schedules, hospitals can tap into a broader segment of the nursing workforce, expanding float pool capacity without increasing full-time headcount or escalating labor costs. It’s a scalable way to boost coverage while supporting a more diverse and adaptable workforce.
3. Supports Nurse Retention
Rigid scheduling is a major driver of nurse burnout and turnover, especially in float pools, where last-minute assignments increase stress and fatigue. Flexible scheduling gives float nurses control over their time, helping them manage responsibilities, avoid high-acuity overload, and maintain work-life balance. This leads to higher satisfaction, stronger retention, and long-term engagement in the float pool.

4 Tips for Nurse Float Pool Optimization
To fully leverage float pools and meet today’s workforce demands, hospitals need a strategic approach. The following four tactics—centralized management, smart technology, predictive tools, and streamlined onboarding—can help maximize float pool efficiency, reduce costs, and improve care coverage system-wide.
1. Centralized Float Pool Management
Consolidating your float pool scheduling and oversight across units or facilities enables better visibility and utilization of your float resources. Centralized management helps allocate staff equitably and efficiently, reducing fragmentation and duplicate efforts common in decentralized models.
2. Utilize Shift Matching Technology
Shift matching technology uses AI to optimize float pool scheduling, improving coverage, reducing overtime, and increasing staff satisfaction. It matches nurses to units based on skills, credentials, availability, preferences, and real-time care needs, making float deployment more efficient and ensuring consistent, high-quality care.
3. Leverage Predictive Scheduling
Adopt data-driven scheduling platforms that forecast upcoming staffing needs and proactively deploy float nurses. Predictive technology reduces last-minute scrambling and reliance on costly overtime or agency staff, improving staff satisfaction and budget control.
4. Streamline Credentialing and Onboarding
Implement fast-track onboarding and maintain up-to-date credential databases for float staff. Efficient credentialing processes reduce delays in making float nurses available and ensure they meet compliance requirements across units.
Strategic Float Pool Management Starts With ShiftMed
ShiftMed delivers a customizable technology-driven solution that empowers your health system to transform its float pools into a scalable, cost-efficient, high-performing workforce asset. Here’s how:
End-to-End Float Pool Management
Manage internal and external workforce resources seamlessly through one unified platform. Eliminate silos, simplify coordination, and unlock scheduling visibility across your system.
Real-Time Scheduling Intelligence
Leverage AI-driven insights to forecast demand, optimize shift coverage, and proactively deploy nurses where needed most before gaps occur.
Credentialing and Compliance at Scale
Accelerate onboarding and maintain compliance across all facilities with centralized, automated credential management—no bottlenecks, no delays.
Local Clinical Support as Needed
Access local, credentialed ShiftMed nurses to quickly backfill shifts as needed without the high cost of traditional travel contracts or agencies.
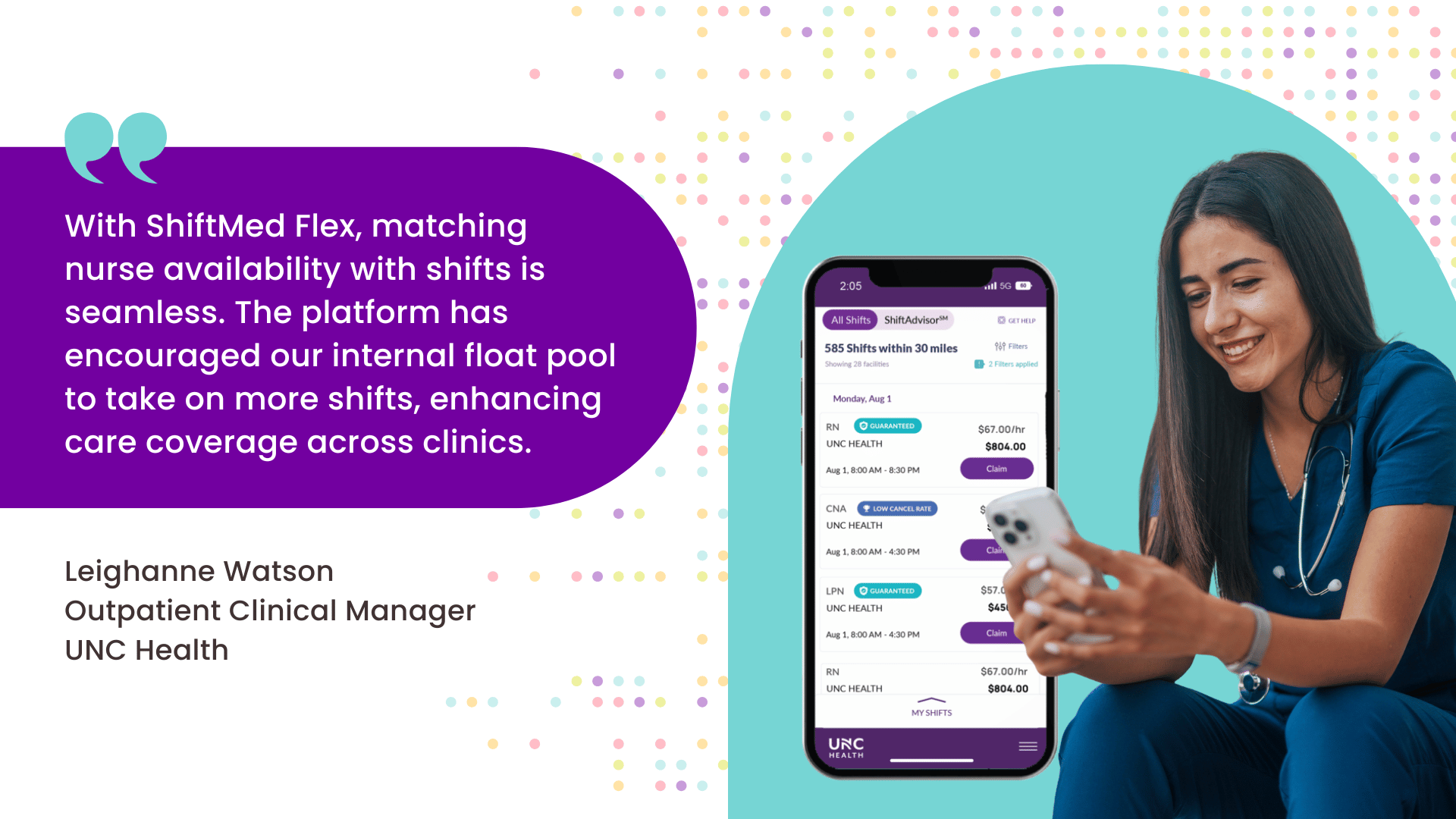
Success Story: UNC Health Doubles Float Pool Engagement
UNC Health, a leading system serving all 100 counties in North Carolina, faced chronic staffing gaps across 258 outpatient clinics due to low float pool participation, which drains full-time staff and impacts care delivery.
To solve this, UNC Health launched ShiftMed Flex in November 2024. This solution gives float nurses real-time visibility into open shifts and full control over when and where they work. The result? A dramatic surge in engagement.
In just 90 days, monthly shift commitments from float nurses doubled— from 4 to 8 per nurse—boosting coverage, relieving core staff, and restoring operational stability. For healthcare executives, this is tech-enabled workforce optimization that delivers measurable impact—fast.
Schedule a workforce consultation and request the ShiftMed Float Pool Optimization Playbook.
The Future of Float Pool Success Starts Now
Float pools are no longer a backup plan but a strategic asset in today’s healthcare workforce landscape. Hospitals that embrace flexible scheduling, centralized management, and data-driven tools can transform underused float pools into reliable, cost-effective coverage engines.
With ShiftMed’s end-to-end platform, hospitals and healthcare systems gain the visibility, agility, and clinical support they need to scale their float pools and protect patient care. Now is the time to reimagine float pool management to fill shifts and build a smarter, more resilient workforce.